Cirrhosis
Condition Basics
What is cirrhosis?
Cirrhosis is a very serious condition in which scarring damages the liver. This scar tissue prevents the liver from working as it should. That can cause problems with blood clotting, which can lead to bleeding and bruising. Cirrhosis can also cause fluid buildup in the belly, jaundice, and severe bleeding in the digestive tract.
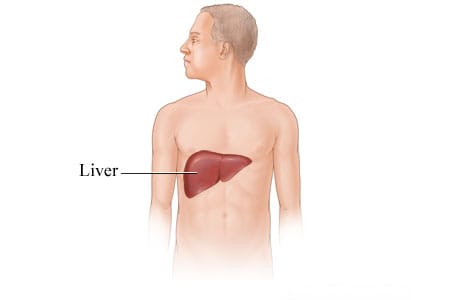
The liver is a large organ in the right upper part of the abdomen. It performs a range of complex and important functions that affect all body systems. Some of the specific functions of the liver include:
- Controlling the amounts of sugar (glucose), protein, and fat entering the bloodstream.
- Removing bilirubin, ammonia, and other toxins from the blood. Bilirubin is a by-product of the breakdown of hemoglobin from red blood cells.
- Processing most of the nutrients absorbed by the intestines during digestion and converting those nutrients into forms that can be used by the body. The liver also stores some nutrients, such as vitamin A, iron, and other minerals.
- Producing cholesterol, substances that help blood clot, bile, and certain important proteins, such as albumin.
- Breaking down (metabolizing) alcohol and many drugs.
What causes it?
Cirrhosis can have many causes. Long-term, heavy use of alcohol can cause cirrhosis. So can chronic viral hepatitis. Other causes include autoimmune diseases, nonalcoholic steatohepatitis (NASH), blocked bile ducts in the liver, and certain diseases.
What are the symptoms?
You may not have symptoms in the early stages of cirrhosis. But as it gets worse, symptoms may include fatigue, yellowing of the skin (jaundice), small red spots and tiny lines on the skin, bruising easily, weight loss, itching, belly pain, and bleeding in the digestive tract.
How is it diagnosed?
The doctor will examine you and ask questions about your symptoms and past health. If the doctor thinks that you might have cirrhosis, you may have blood tests and imaging tests, such as an ultrasound or a CT scan. To confirm that you have cirrhosis, the doctor may do a liver biopsy.
How is cirrhosis treated?
Treatment may include medicines, surgery, or lifestyle changes. Treatment can't cure cirrhosis. But it can sometimes prevent or delay more liver damage. To limit the damage to your liver and help control symptoms, you can make lifestyle changes. For example, don't drink alcohol. Limit sodium and fat. And avoid medicines that can harm your liver.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
Cirrhosis can have many causes. Some of the main ones include:
- Long-term, heavy use of alcohol.
- Chronic viral hepatitis.
- Autoimmune diseases. These include autoimmune hepatitis and primary sclerosing cholangitis (PSC).
- Nonalcoholic fatty liver disease (NAFLD), such as nonalcoholic steatohepatitis (NASH). This is the buildup of fat in liver cells.
- Blocked bile ducts. The ducts that carry bile out of the liver can get inflamed and blocked. This causes a disease called primary biliary cholangitis.
- Certain diseases that run in families. These include Wilson's disease, cystic fibrosis, and hemochromatosis.
Less common causes include severe reactions to medicines. Cirrhosis may also be caused by long-term exposure to poisons, such as arsenic. Some people have it without a clear cause.
Learn more
Symptoms
You may not have symptoms in the early stages of cirrhosis. But as it gets worse, it can cause a number of symptoms. These include:
- Fatigue.
- Small red spots and tiny lines on the skin, called spider angiomas.
- Bleeding problems, such as bruising easily or heavy nosebleeds.
- Weight loss.
- Yellowing of the skin (jaundice).
- Itching.
- Swelling from fluid buildup in the legs (edema) and the belly (ascites).
- Bleeding from enlarged veins in the digestive tract.
- Confusion.
Scar tissue from cirrhosis may block the proper flow of blood from the intestines through the liver. The scarring can lead to increased pressure in the veins that supply this area. This is called portal hypertension. It can lead to other health complications.
Learn more
When to Call a Doctor
Call 911 anytime you think you may need emergency care. For example, call if:
- You have trouble breathing.
- You vomit blood or what looks like coffee grounds.
Call your doctor now or seek immediate medical care if:
- You feel very sleepy or confused.
- You have new or worse belly pain.
- You have a fever.
- There is a new or increasing yellow tint to your skin or the whites of your eyes.
- You have any abnormal bleeding, such as:
- Nosebleeds.
- Vaginal bleeding that is different (heavier, more frequent, at a different time of the month) than what you are used to.
- Bloody or black stools, or rectal bleeding.
- Bloody or pink urine.
Watch closely for changes in your health, and be sure to contact your doctor if:
- You have any problems.
- Your belly is getting bigger.
- You are gaining weight.
Exams and Tests
Your doctor will do a physical exam and ask about your medical history to see if you have symptoms of liver disease and to help find out possible causes of liver damage.
If your doctor thinks that you might have cirrhosis, you may have blood and imaging tests. You also may have a liver biopsy. This test can show for sure if you have cirrhosis.
Blood tests to check liver function
Measuring the levels of certain chemicals produced by the liver can show how well your liver is working. Blood tests may be used to measure:
- Albumin and total serum protein. Albumin is a type of protein. Liver disease can cause a decrease in protein levels in the blood.
- Partial thromboplastin time or prothrombin time/INR. These tests measure blood-clotting factors that are produced in the liver.
- Bilirubin. This is produced when the liver breaks down hemoglobin, the substance in red blood cells that carries oxygen. Cirrhosis may cause high bilirubin levels, which causes jaundice.
Blood tests to check for inflammation of the liver
You may have blood tests to check your liver enzymes. These can help show if you've had liver inflammation for a long time. These blood tests include:
- Aspartate aminotransferase (AST), alanine aminotransferase (ALT), and lactate dehydrogenase (LDH). An increased level of these enzymes may mean injury to the liver and the death of liver cells.
- Alkaline phosphatase (ALP). An increased ALP level may mean that the bile ducts are blocked.
- Gamma glutamyl transferase (GGT), also called gamma-glutamyl transpeptidase (GGTP). An increased level can happen because of alcohol use or diseases of the bile ducts.
Some people with cirrhosis have normal liver enzymes.
Tests that show an image of the liver
Imaging tests can check for tumors and blocked bile ducts. They also can be used to look at the size of the liver and to see how blood flows through the liver. These tests include:
- Abdominal ultrasound.
- CT scan of the abdomen.
- MRI scan of the abdomen.
- Liver and spleen scan.
Learn more
Watch
Treatment Overview
Treatment may include medicines, lifestyle changes, and regular doctor visits. In some cases, you may need surgery to treat complications from cirrhosis. Your treatment depends on the cause of your cirrhosis and what other problems it is causing.
Treatment can't cure cirrhosis. But it can sometimes prevent or delay more liver damage.
Lifestyle changes
Your doctor will recommend some lifestyle changes to help prevent more liver damage.
- Do not drink any alcohol. If you don't stop completely, liver damage may quickly get worse.
- Talk to your doctor before you take any prescription or over-the-counter drugs, vitamins, supplements, or herbs. Medicines that can hurt your liver include acetaminophen (such as Tylenol) and other pain medicines such as aspirin, ibuprofen (such as Advil or Motrin), and naproxen (Aleve).
- Follow a low-sodium and low-fat diet. Cutting back on sodium can help prevent fluid buildup in your belly and chest.
Immunizations
- Get immunized. This includes vaccines against hepatitis A and hepatitis B, influenza, shingles, and pneumococcus.
Treatment for complications of cirrhosis
Cirrhosis can cause other problems (complications) that may need treatment. They include:
- Fluid buildup in the belly (ascites). It can be serious if it isn't controlled. Treatment may include:
- Following a low-sodium diet.
- Taking medicines such as diuretics and antibiotics.
- Removing fluid with a needle (paracentesis).
- Getting a transjugular intrahepatic portosystemic shunt (TIPS). This diverts fluid from the belly.
- Bleeding from enlarged veins. Variceal bleeding in the digestive tract can be treated with:
- Beta-blocker and vasoconstrictor medicines.
- Shunts to move blood or other fluid away from the belly.
- Endoscopic variceal banding or sclerotherapy to stop bleeding.
- Balloon tamponade. A doctor inserts and inflates a balloon in the lower part of the esophagus or upper part of the stomach. This stops bleeding by pressing against the veins.
- Changes in mental function. Encephalopathy may occur when the liver can't filter poisons from the bloodstream. As these toxins build up in your blood, they can affect your brain function. You may need to:
- Take lactulose. This medicine helps prevent the buildup of ammonia and other toxins in the large intestine.
- Avoid sedative medicines, such as sleeping pills, medicines for anxiety, and opioids. These can make symptoms of encephalopathy worse.
Liver transplant
Receiving a liver from an organ donor (liver transplant) is the only treatment that will restore normal liver function and cure portal hypertension. A liver transplant is usually an option only when liver damage is severe and threatening your life.
Before your condition becomes severe, you may want to talk to your doctor about whether you'll be a good candidate for a liver transplant if your disease gets worse.
Talk to your doctor about what steps you can take now to improve your overall health. That way you can increase your chances of being considered a good candidate.
Learn more
- Cirrhosis: Beta-Blockers for Portal Hypertension and Varices
- Cirrhosis Complications: Variceal Bleeding
- Cirrhosis: Surgical Shunts for Portal Hypertension
- Cirrhosis: Vasoconstrictor Medicines for Variceal Bleeding
- Endoscopic Treatment for Variceal Bleeding
- Organ Transplant
- Paracentesis
- Transjugular Intrahepatic Portosystemic Shunt (TIPS)
Self-Care
Lifestyle changes may reduce symptoms caused by complications of cirrhosis. These changes may also help to slow new liver damage.
Giving up alcohol
If you have cirrhosis, it's important that you stop drinking alcohol completely, even if alcohol wasn't the cause of the cirrhosis. If you don't stop, liver damage may quickly get worse.
Changing your diet
You may need to limit the amount of salt you eat.
If your body is retaining fluid, you'll need to reduce your sodium intake. You do this by reducing the amount of salt in your diet. People with liver damage tend to retain sodium. This can make fluid build up in your belly (ascites).
Your doctor may also talk to you about changing your diet. Certain foods may make symptoms worse.
Avoiding harmful medicines
Some medicines should be used carefully or not taken at all if you have cirrhosis. For example, acetaminophen (such as Tylenol) can speed up liver damage. Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) increase the risk of variceal bleeding if you have enlarged veins (varices) in the digestive tract. NSAIDs can also raise your risk for ascites. They include ibuprofen (such as Motrin or Advil) and naproxen (Aleve). Talk to your doctor or pharmacist about what medicines are safe for you.
Certain prescription medicines used to treat other conditions may be harmful if you have cirrhosis. Make sure that your doctor knows all the medicines you take (including all nonprescription medicines, vitamins, herbs, and supplements).
Improving your general health
Taking other steps to improve your overall health may help you cope with the symptoms of cirrhosis.
- Stop smoking. Quitting tobacco use will improve your overall health. This may help make you a better candidate for a liver transplant if you need one.
- Take a multivitamin if your doctor recommends it. Don't take one that contains extra iron unless your doctor tells you to. And don't take an iron supplement unless your doctor recommends it.
- Brush and floss your teeth daily. This helps avoid dental problems that could lead to infection (abscess). Be gentle when you floss so you don't make your gums bleed.
- Make sure you have been vaccinated against:
- Influenza (flu). Get a flu shot every year. People with cirrhosis are at increased risk for serious complications from the flu.
- COVID-19. Stay up to date on your COVID-19 vaccines.
- Hepatitis A and hepatitis B.
- Pneumococcus. It can cause pneumonia or abdominal infection (peritonitis). Ask your doctor how often you should be revaccinated.
- Shingles.
Using complementary and alternative medicines wisely
In general, you should avoid most herbal and other supplements. They may make liver disease worse.
Talk to your doctor about whether you should try any alternative treatment.
Learn more
Watch
Related Information
Credits
Current as of: October 19, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: October 19, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.