Low Back Pain
Condition Basics
What is low back pain?
Low back pain is pain that can occur anywhere below the ribs and above the legs. It is very common. Almost everyone has it at one time or another.
Low back pain can be:
- Acute. This is new pain that can last a few days to a few weeks—at the most a few months.
- Chronic. This pain can last for more than a few months. Sometimes it can last for years.
What causes it?
Causes of low back pain may include overuse, injury, illness, or changes that happen with age, such as arthritis. In most cases, it's not clear what causes low back pain.
What are the symptoms?
Low back pain may be dull or sharp. It may be in one small area or over a broad area. You may also have muscle spasms, numbness, tingling, or weakness in one or both legs.
How is it diagnosed?
Your doctor will do a physical exam and ask questions about your back and overall health. Most people don't need any tests right away. But if your pain lasts more than 6 weeks, your doctor may order an X-ray, a CT scan, or an MRI.
How is low back pain treated?
Most low back pain improves with self-care. This includes ice or heat and light activity such as walking. Use over-the-counter pain medicine as needed.
For severe symptoms or pain that continues after 2 weeks of self-care, see your doctor. You may benefit from other treatment, such as stronger medicine, exercises, or manual therapy.
There are a number of other treatments for back pain. You may need to try more than one to see what works best for you. Common treatments include acupuncture, massage, and yoga.
For chronic back pain, one type of treatment by itself may not help. The best plan is often a mix of treatments.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
In most cases, there isn't a clear cause. Some causes of low back pain are:
- Injury or overuse.
- This can include fractures or compression fractures of bones, sprains or strains of soft tissues such as ligaments and muscles, or injuries to the small joints between the bones of the spine.
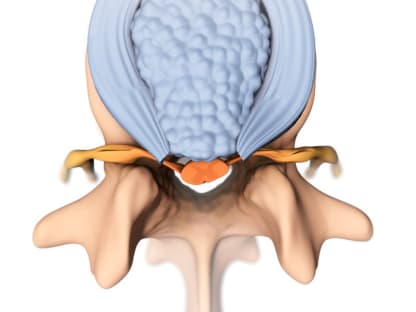
- Pressure on nerve roots.
- Conditions such as a herniated disc or spinal stenosis can cause this kind of pressure.
- Osteoarthritis.
- This type of arthritis is usually caused by getting older.
- When arthritis affects the small joints in the spine, it can lead to back pain by making the joints themselves stiff and sore. It can also create pressure on the nerve roots.
- Arthritis in other joints, such as the hips, can cause you to limp or to change the way you walk. This can also lead to back pain.
Less common spinal conditions that can cause low back pain include:
- Ankylosing spondylitis. This is a form of arthritis that most often affects the spine.
- Bacterial infection in the bone, spinal discs, or spinal cord.
- Spinal tumors. These can be growths on the bones and ligaments of the spine, on the spinal cord, or on nerve roots.
What Increases Your Risk
You're more likely to have low back pain if:
- You're overweight. Excess body weight, especially around the waist, may put strain on your back.
- You've had a previous back injury or back surgery.
- You've had compression fractures of the spine.
- You're pregnant.
Other things that may put you at risk include:
- Lack of regular exercise.
- If you're not active, the muscles and joints in your back can get weak and stiff.
- Job duties or other activities.
- Jobs or activities that require long periods of sitting, lifting heavy objects, bending or twisting, repetitive motions, or constant vibration can strain your back.
- Smoking.
- People who smoke are more likely to have disc injuries than people who don't smoke.
- Poor posture.
- After your back has been strained or injured, bad posture can make your pain worse.
- Having a disease or illness that causes chronic coughing.
- Chronic coughing puts lots of stress on your spine.
Prevention
There are some things you can do that may help prevent low back pain. And they can prepare you for a faster recovery if you do have low back pain.
- Exercise and be active to keep your back healthy and strong.
- Learn how to lift objects safely to protect your back.
- Practice good posture, whether you are sitting or standing.
- Try different sleeping positions that protect your back.
- Wear low-heeled shoes.
- Stay at a healthy weight to avoid excess strain on your lower back.
- If you smoke, quit.
- Eat a healthy diet.
- Manage your stress.
But there is no clear evidence that you can prevent low back pain or keep it from coming back.
Learn more
Watch
Symptoms
Back pain can come on quickly or over time. You may feel:
- Pain in your hips or buttock.
- Leg pain, numbness, tingling, or weakness. When a nerve gets squeezed—such as from a disc problem or arthritis—you may have symptoms in your leg or foot. You can even have leg symptoms from a back problem without having any pain in your back.
- Pain that's sharp or dull, sometimes with stiffness or muscle spasms. It may be in one small area or over a broad area. But even bad pain doesn't mean that it's caused by something serious.
What Happens
The course of low back pain depends both on its cause and on how well you treat your back.
Most back pain gets better within 4 to 6 weeks with some basic self-care. But for some people, the pain lasts longer.
Chronic back pain is pain that has lasted longer than 3 months. This kind of back pain not only wears you down, but it also can trigger other problems. If your back pain causes you to use your body in different ways (for example, to limp or to sit differently), pain can develop in other areas of your body. Pain can also cause changes in your body that tend to keep the pain going.
Chronic back pain can be difficult to treat. But by working with a doctor and trying different treatments, most people can find relief.
Watch
When to Call a Doctor
Call 911 or other emergency services immediately if:
- Back pain occurs with chest pain or other symptoms of a heart attack.
- A person has signs of damage to the spine after an injury (such as a car crash, fall, or direct blow to the spine). Signs may include:
- Being unable to move part of the body.
- Severe back or neck pain.
- Weakness, tingling, or numbness in the arms or legs.
Call your doctor now if:
- You have new or worse numbness in your legs.
- You have new or worse weakness in your legs. (This could make it hard to stand up.)
- You have a new loss of bowel or bladder control.
- You have new or increased back pain with fever, painful urination, or other signs of a urinary tract infection.
- You have long-term back pain that suddenly gets much worse, and you didn't cause it by being more active.
- You have a history of cancer or HIV infection, and you have new or increased back pain.
- Pain wakes you from sleep.
Watchful waiting
Most low back pain doesn't require a visit to a doctor.
If the pain doesn't get better after 1 or 2 days and you can't do your normal daily activities, call your doctor.
If you still have mild to moderate pain after at least 2 weeks of home treatment, talk with your doctor. You may need to be checked for problems that may be causing your back pain.
Check your symptoms
Exams and Tests
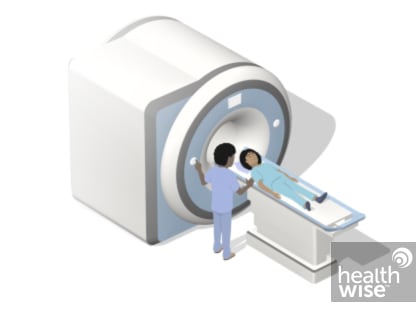
A physical exam is the main way to diagnose low back pain. Your doctor may examine your back, check your nerves by testing your reflexes, and make sure that your muscles are strong. Your doctor also will ask questions about your back and overall health.
Most people don't need any tests right away. Tests often don't show the reason for your pain.
If your pain lasts more than 6 weeks or you have symptoms that your doctor is more concerned about, then your doctor may order tests. These may include an X-ray, a CT scan, or an MRI. Sometimes other tests such as a bone scan or nerve conduction test may be done.
Learn more
Watch
Treatment Overview
Most acute low back pain gets better on its own within several weeks, no matter what the cause. Time and doing usual activities are all that most people need to feel better.
Using heat or ice and taking over-the-counter pain medicine also can help while your body heals.
If you aren't getting better on your own or your pain is very bad, your doctor may recommend:
- Physical therapy.
- Spinal manipulation, such as by a chiropractor.
- Acupuncture.
- Massage.
- Injections of steroid medicine in your back (especially for pain that involves your legs).
If you have chronic low back pain, treatment will help you understand and manage your pain. Treatment may include:
- Staying active. This may include walking or doing back exercises.
- Physical therapy.
- Medicines. Some of these medicines are also used for other problems, like depression.
- Pain management. Your doctor may have you see a pain specialist.
- Counseling. Having chronic pain can be hard. It may help to talk to someone who can help you cope with your pain.
Surgery isn't needed for most people. But it may help some types of low back pain.
Learn more
Watch
Self-Care
Almost everyone has low back pain at some time. The good news is that most low back pain will go away in a few days or weeks with some basic self-care.
Some people are afraid that doing too much may make their pain worse. In the past, people stayed in bed, thinking this would help their backs. Now doctors think that, in most cases, getting back to your normal activities is good for your back, as long as you avoid doing things that make your pain worse.
Ease back into daily activities
- For the first day or two of pain, take it easy. But as soon as you can, get back to your normal daily life and activities.
- Get gentle exercise, such as walking. Movement keeps your spine flexible and helps your muscles stay strong.
- If you are an athlete, return to your activity carefully. Choose a low-impact option until your pain is under control.
Avoid or change activities that cause pain
- Try to avoid too much bending, heavy lifting, or reaching. These movements put extra stress on your back.
- In bed, try lying on your side with a pillow between your knees. Or lie on your back on the floor with a pillow under your knees.
- When you sit, place a small pillow, a rolled-up towel, or a lumbar roll in the curve of your back for extra support.
- Try putting one foot up on a stool or changing positions every few minutes if you have to stand still for a period of time.
Pay attention to body mechanics and posture
Body mechanics are the way you use your body. Posture is the way you sit or stand.
- Take extra care when you lift. When you must lift, bend your knees and keep your back straight. Avoid twisting, and keep the load close to your body.
- Stand or sit tall, with your shoulders back and your stomach pulled in to support your back.
Get support when you need it
- Let people know when you need a helping hand. Get family members or friends to help out with tasks you can't do right now.
- Be honest with your doctor about how the pain affects you.
- If you've had to take time off work, talk to your doctor and boss about a gradual return-to-work plan. Find out if there are other ways you could do your job to avoid hurting your back again.
Reduce stress
Worrying about the pain can cause you to tense the muscles in your lower back. This in turn causes more pain. Here are a few things you can do to relax your mind and your muscles:
- Take 10 to 15 minutes to sit quietly and breathe deeply. Try to focus only on your breathing. If you can't keep thoughts away, think about things that make you feel good.
- Get involved in your favorite hobby, or try something new.
- Talk to a friend, read a book, or listen to your favorite music.
- Find a counselor you like and trust. Talk openly and honestly about your problems. Be willing to make some changes.
Learn more
- Back Problems: Proper Lifting
- Back School for Low Back Pain
- Get Chores Done Without Making Your Pain Worse
- Pain: Getting Help at Home
- Low Back Pain and Sex
- Low Back Pain: Easing Back Into Your Daily Activities
- Low Back Pain: Exercises to Reduce Pain
- Returning to Work With Low Back Pain
Hear from others
Watch
Medicines
Medicine can help relieve low back pain and reduce muscle spasms in some people. But medicine alone doesn't work well to treat low back pain. It should be used along with other treatments, such as walking and using heat or ice.
Medicines that work for some people don't work for others. Let your doctor know if the medicine you take doesn't work for you. You may be able to take another medicine for your back pain.
Medicine choices
Your doctor may recommend several medicines, depending on how long you've had pain, what other symptoms you have, and your past health.
The medicines suggested most often are:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen.
-
These seem to be the over-the-counter pain relievers that work best for low back pain. But if you can't take NSAIDs, you can try acetaminophen instead. You can buy these kinds of medicines without a prescription. Some of them also come in stronger doses. For those, you'll need a prescription.
- Muscle relaxers.
-
These medicines can help with severe muscle spasms that happen when the back pain starts (acute phase). Side effects are common. For example, you may feel drowsy.
- Opioid pain relievers.
-
These are very strong medicines. They are sometimes used when other medicines don't help your pain. They are usually taken for only a few days.
- Antidepressants.
-
Some of these medicines, such as duloxetine, not only treat depression but also may help with chronic pain.
Other medicines are sometimes used for low back pain. They include:
- Anesthetic or steroid injections.
-
These injections don't seem to help most people with chronic back pain. They may give short-term relief to some people with leg pain from a back problem.
- Botox injection.
-
This is a shot into the back muscles. It hasn't been well tested for chronic low back pain.
Learn more
Watch
Surgery
When you're in a lot of pain, you might wonder if you need surgery to fix what's wrong so that you can feel better.
Every case is different. But most people don't need surgery for low back pain.
When surgery may help
Reasons for having surgery for low back pain include:
- You have nerve pain from herniated discs. This is why most back surgeries are done. The disc problem causes pain in your leg that prevents you from doing everyday tasks. You may have pain, numbness, or tingling through your buttock and down the back of your leg (sciatica) or in the front of your thigh.
- A spinal fracture caused by an injury.
- An infection in your spine.
- A problem that causes your spine to be unstable.
- A tumor in your spine.
- Spinal stenosis. This is the narrowing of the spinal canal.
- Loss of feeling or weakness in your back or legs that gets worse over time.
- Loss of control of your bowel or bladder.
Back surgery doesn't always work. Depending on the condition, you may still have back pain after surgery.
A rehabilitation program is very important after most back surgery. If you can't or won't commit to physical therapy after surgery, you may not be a good candidate for surgery.
Surgery choices
There are several types of back surgery. Some, like a discectomy, can help people who have severe symptoms. Others have not been proved to work.
If you do need surgery, you and your doctor will decide which type is best for you. Having surgery for a herniated disc or another back problem is a big decision.
Types of surgeries include:
- Discectomy for a herniated disc. This removes the herniated disc material that is causing the problem.
- Laminectomy for spinal stenosis. This surgery relieves pressure on the spinal cord nerve roots.
- Kyphoplasty and vertebroplasty. These surgeries are done to try to relieve pain from compression fractures of the spine.
- Surgeries for tumors and infection.
- Spinal fusion. This is surgery to join, or fuse, two or more vertebrae in the low back.
Learn more
- Decompressive Laminectomy for Lumbar Spinal Stenosis
- Discectomy for a Lumbar Herniated Disc
- Intradiscal Electrothermal Therapy (IDET) for Low Back Pain
- Kyphoplasty
- Lumbar Herniated Disc: Should I Have Surgery?
- Lumbar Spinal Fusion (Arthrodesis)
- Percutaneous Discectomy for a Lumbar Herniated Disc
Hear from others
Watch
Complementary Treatments
You can choose from a number of alternative treatments for your low back pain. Because some of these treatments are new or aren't yet well researched, they may not be covered by health insurance.
- Massage may reduce low back pain for a short time. It is likely to work best if you also learn to do exercises for your back and learn the best ways to lift and move to protect your back.
- Biofeedback may provide short-term pain relief, but there isn't enough evidence to show it will help.
- Acupuncture may help reduce pain and allow you to be active for a short time after treatment, but not any more than other treatments.footnote 1
- Acupressure uses pressure on certain points in the body to decrease symptoms. Small studies suggest that it reduces pain and allows a person to be more active.footnote 2
- Relaxation techniques can help reduce muscle tension, stress, and depression.
- Yoga is another way to stay active and get help with relaxation and managing stress. There is some evidence that yoga may help people with chronic low back pain to control their symptoms and stay more active. But it's not clear if yoga is more helpful than any other activity or treatment for chronic low back pain.footnote 3 There are different types of yoga. Talk to your doctor before you start a yoga program.
- Capsaicin cream may help relieve pain.footnote 4 It's a substance contained in cayenne peppers. Capsaicin cream is put on the skin over the painful area.
- Transcutaneous electrical nerve stimulation (TENS) gives brief pulses of electricity to nerve endings in the skin to relieve pain.
Learn more
Watch
Related Information
References
Citations
- Mu J, et al. (2020). Acupuncture for chronic nonspecific low back pain. Cochrane Database of Systematic Reviews, 12: CD013814. DOI: 10.1002/14651858.CD013814. Accessed March 25, 2021.
- Hsieh LL, et al. (2006). Treatment of low back pain by acupressure and physical therapy: Randomised controlled trial. BMJ, 333(7543): 696–700.
- Wieland LS, et al. (2022). Yoga for chronic non-specific low back pain. Cochrane Database of Systematic Reviews, 11(11): CD010671. DOI: 10.1002/14651858.CD010671.pub3. Accessed February 8, 2023
- Gagnier JJ, et al. (2016). Herbal medicine for low back pain: A Cochrane review. Spine, 41(2): 116–133. DOI: 10.1097/BRS.0000000000001310. Accessed June 17, 2016.
Credits
Current as of: July 24, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 24, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.